Neurologijos seminarai ISSN ISSN 1392-3064 / eISSN 2424-5917
2023, 27(98), pp. 261–266 DOI: https://doi.org/10.15388/NS.2023.27.98.1
Klinikinis atvejis / Case Report
S. Radzevičiūtė*
Faculty of Medicine, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania
G. Liaudanskytė
Faculty of Medicine, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania
I. Baužaitė
Faculty of Medicine, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania
N. Balčiūnienė
Department of Neurosurgery, Neurosurgery Intensive Care Unit, Lithuanian University of Health Sciences, Kaunas, Lithuania
A. Vaitkus
Department of Neurology, Lithuanian University of Health Sciences, Kaunas, Lithuania
Summary. The frequency of brain abscesses is rising, and they continue to be a potentially fatal infection. It may result from an infection source spreading nearby or over great distances. Additionally, immunocompromised patients – including those who have had immunomodulating treatments – represent a significant risk factor for brain abscesses. The presenting signs of brain abscess are variable and nonspecific. Patients most commonly are presented with headache, fever, altered mental status, focal neurologic symptoms, nausea and vomiting. Healthcare providers must maintain a high degree of clinical suspicion for early diagnosis in immunosuppressed patients because of their diminished capacity to generate a typical immune response, which can make typical infection indications less obvious. Brain imaging is critical to improving the prognosis and is necessary for the diagnosis and treatment of brain abscesses. Magnetic resonance imaging (MRI) remains the preferred radiologic method for diagnosis and differentiation. The proper handling of brain abscess samples is crucial for the correct reporting of microbiological findings. In immunocompetent individuals, the best empirical antibiotic therapy for a community-acquired brain abscess is a combination of metronidazole and a third-generation cephalosporin, whereas, in patients with severe immunodeficiency, trimethoprim-sulfamethoxazole and voriconazole should be added. Still, surgical excision or draining of the abscess is the recommended course of treatment, followed by long-term antibiotics. In this article, we present a patient who was diagnosed with brain abscess and treated non-surgically; as also, a multidisciplinary approach of medical care was followed.
Keywords: brain abscess, immunosuppression, myasthenia gravis
Santrauka. Galvos smegenų abscesai yra dažna mirtina infekcija. Ši patologija gali atsirasti dėl infekcijos židinio plitimo. Be to, imunosupresija, įskaitant imunosupresinių vaistų vartojimą, yra reikšmingas galvos smegenų abscesų rizikos veiksnys. Smegenų absceso pradiniai požymiai yra nespecifiški, pacientai dažniausiai kreipiasi dėl galvos skausmo, karščiavimo, pykinimo ir vėmimo, pakinta jų psichinė būsena ar atsiranda židininių neurologinių simptomų. Ankstyva diagnostika yra gyvybiškai svarbi pacientams ir didina išgyvenamumo tikimybę. Imunosupresijos būklės pacientams sumažėjęs imuninis atsakas gali maskuoti tipinius infekcijos požymius ir simptomai tampa mažiau akivaizdūs. Galvos smegenų vaizdiniai tyrimai yra kritiškai svarbūs gerinant prognozę ir būtini diagnozuojant bei gydant galvos smegenų abscesus. Magnetinio rezonanso tomografija (MRT) tebėra pagrindinis radiologinis diagnozės nustatymo ir diferenciacijos nuo galvos smegenų navikų metodas. Infekcijos sukėlėjui išaiškinti svarbu paimti pasėlį iš esamo židinio. Imunosupresiją patiriantiems asmenims geriausia empirinė antibiotikų terapija smegenų abscesui gydyti yra metronidazolio ir trečiosios kartos cefalosporino derinys, o pacientams, kuriems yra sunkus imunodeficitas, turėtų būti pridėti trimetoprimas-sulfametoksazolas ir vorikonazolas. Vis dėlto rekomenduojamas gydymas yra chirurginis absceso pašalinimas arba drenažas, paskui ilgą laiką reikia vartoti antibiotikus. Šiame straipsnyje pristatome klinikinį atvejį pacientės, kuriai buvo nustatytas galvos smegenų abscesas (jis buvo gydytas konservatyviai) ir daugiadalykės komandos svarbą diagnozuojant ir gydant šią mirtiną patologiją.
Raktažodžiai: smegenų abscesas, imunosupresija, sunkioji miastenija.
_______
* Address: Silvija Radzevičiūtė, Department of Neurosurgery, Neurosurgery Intensive Care Unit, Lithuanian University of Health Sciences, Kaunas, Lithuania, Eivenių 2, LT-50161, Kaunas. Tel. (+370) 69524378, e-mail: silvradz1118@kmu.lt
Received: 02/02/2024. Accepted: 23/02/2023
Copyright © Silvija Radzevičiūtė, Gabija Liaudanskytė, Ieva Baužaitė, Neringa Balčiūnienė, Antanas Vaitkus, 2023. Published by Vilnius University Press.This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Brain abscess is a potentially fatal illness which needs to be treated urgently. It is challenging to diagnose this condition early due to its nonspecific symptoms. Healthcare providers must maintain a high degree of clinical suspicion for early diagnosis in immunosuppressed patients because of their diminished capacity to generate a typical immune response, which can make typical infection indications less obvious. There has been progress in the detection and treatment of brain abscesses, but the accompanying morbidity and fatality rate is still quite high.
This case report presents a patient who was transported to the hospital following an accident at home, caused by dizziness she experienced before. Head computed tomography (CT) was performed, which showed multiple lesions in her brain, along with possible brain abscesses. Immunosuppressants were used to treat the patient’s myasthenia gravis, which had been identified eight years prior.
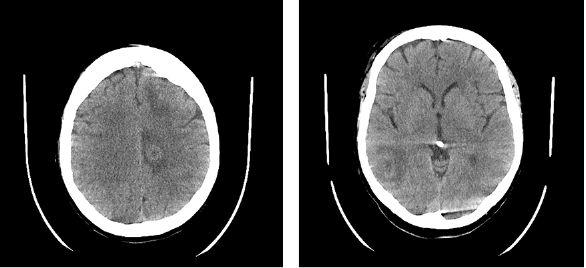
In November 2023, a 55-year-old female patient was hospitalized following a fall at home which resulted in a left elbow fracture. The patient had been feeling dizzy before the incident, prompting a head CT to exclude a head trauma and determine the cause of the dizziness. The CT revealed multiple brain lesions, with differential diagnoses including metastases and abscesses (Fig. 1), necessitating further evaluation via magnetic resonance imaging (MRI). The patient’s medical history indicates that she had been diagnosed with seropositive myasthenia gravis in July 2015. The diagnosis was confirmed by the presence of positive antibodies against acetylcholine receptors (AChR), and a muscle biopsy was performed. The patient was taking Mestinon 60mg x 3, Prednisolone 5mg x 1, and Azathioprine 50mg x 2 for treatment. Plasmapheresis was used to treat exacerbations of myasthenia gravis.
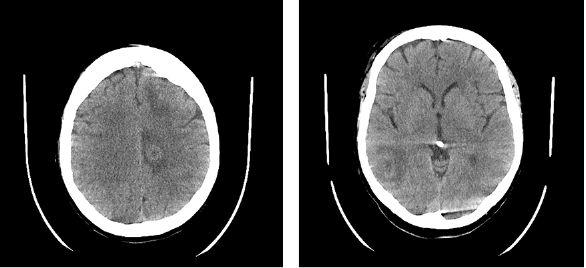
During elbow surgery, the patient experienced respiratory insufficiency, necessitating transfer to the Intensive Care Unit (ICU). Once stabilized, she was moved to the Neurology Department. Subsequent deterioration during a routine morning examination included nausea, diaphoresis, elevated blood pressure (220/90 mmHg), and tachycardia (heart rate 100 bpm). The worsening respiratory insufficiency led to her transfer to the Neurosurgical ICU and subsequent intubation. Despite normal laboratory findings, a chest CT revealed inflammatory infiltration and hypoventilation, but an infection was initially ruled out, precluding antibiotic administration. However, a repeated bronchoscopy culture isolated Proteus Mirabilis, sensitive to Cefuroxime, leading to a diagnosis of respiratory muscle weakness potentially related to myasthenia, and subsequent plasmapheresis was initiated. After extubation and initial stabilization, MRI revealed brain lesions to be consistently recognized as abscesses (Fig. 2).
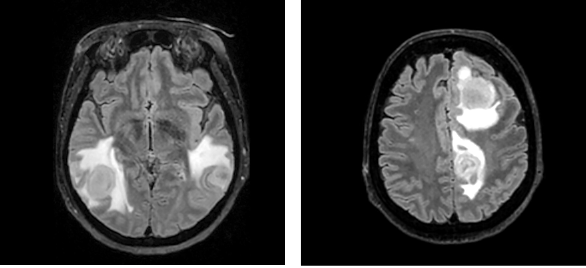
The patient’s condition deteriorated during transportation, requiring re-intubation. Neurosurgical intervention was not considered viable. Consequently, the antibiotic regimen was expanded to include Ceftriaxone, Vancomycin, Metronidazole, and Sulfamethoxazole-Trimethoprim, targeting a broader spectrum of pathogens potentially responsible for brain abscesses. Despite plans to conduct diagnostic tests for HIV, syphilis, toxoplasmosis, and Listeria from the abscess aspirates, the patient’s condition rapidly deteriorated, becoming critically unstable. This acute decline was marked by severe respiratory insufficiency and profound bradycardia, necessitating immediate cardiopulmonary resuscitation (CPR) and the urgent administration of Atropine. Finally, due to prolonged intubation, it was decided to form a tracheostomy. Subsequent MRI showed a reduction in the abscess size (Fig. 3), and the patient was transferred to the Neurology Department for continued care.
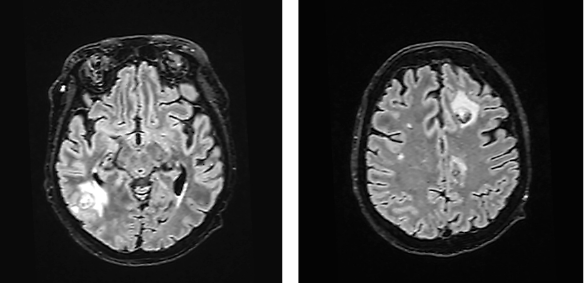
During the consultation in the Neurology Department, it was decided not to perform a puncture of the brain abscesses due to the potential risk of developing secondary meningitis. Antibiotic therapy was continued to cover possible pathogens of the brain abscesses. The patient’s condition and muscle strength improved during the course of treatment. The dynamics of the brain abscesses were positive, and the laboratory inflammation markers decreased. During the course of treatment, the patient had three episodes of loss of consciousness, which were considered to be of epileptic origin. Levetiracetam 750mg/day was prescribed. Antibiotic therapy with Vancomycin, Ceftriaxone, and Metronidazole was ongoing (already in week 15).
Brain abscess has been increasing in incidence. It remains a life-threatening infection, with a 1-year mortality rate of 20% [1]. Ageing populations and an increasing prevalence of immunocompromising conditions combined with improved diagnostics may have contributed to an observed increase in the incidence rate since the 1980s, with a rise from 0.6 to 0.9 per 100,000 per year from 2010 to 2016, as assessed by healthcare registries [2]. This condition may occur at any age, but the majority of cases are manifested between the third and fifth decades of life [3].
Brain abscess can arise from a contiguous (otogenic infection, dental infection, sinusitis or mastoiditis) or from a distant spread of a source of infection (congenital cyanotic cardiomyopathy, endocarditis, pulmonary infection, etc.) [4], a recent neurosurgical procedure or a penetrating head trauma. Endocarditis or pulmonary infections (pneumonia, empyema, and abscess) are the most common sources of hematogenous spread [3]. Moreover, immunocompromise is an important risk factor for brain abscess, including patients who underwent immunomodulating treatments [1]. This population is prone to the spread of infection to the central nervous system, which often originates from a primary infection in the lungs, and can lead to the formation of one or more abscesses. It must be distinguished from toxoplasma encephalitis which is the most common multifocal infectious process encountered in advanced HIV. Individuals with AIDS having brain abscesses are more likely to have multiple abscesses and tuberculous abscesses. This population is also more susceptible to intracranial infection from Listeria, Cryptococcus, and Nocardia [3]
The presenting signs of brain abscess are variable and nonspecific. Patients are most commonly presented with headache, fever, altered mental status, focal neurologic symptoms, nausea and vomiting. Seizures are less common and may have either focal or generalized presentation. Moreover, neck stiffness and meningismus have been reported. Most patients with a brain abscess show unclear and non-specific symptoms, making it crucial for healthcare professionals to maintain a high level of clinical suspicion for early diagnosis. This is particularly important in immunosuppressed individuals. Due to their impaired ability to produce a normal immune response, these patients are more vulnerable, and the usual signs of infection might be less apparent in them [3].
Laboratory data are of limited utility in diagnosis. Leucocytosis and elevation in erythrocyte sedimentation rate are common, but the absence of these laboratory abnormalities will not exclude the diagnosis. Imaging of the brain is essential for the diagnosis and management of brain abscesses and plays a crucial role in enhancing the prognosis. MRI has greater sensitivity and specificity than CT in identifying pyogenic infection [3]. Distinguishing an abscess from a metastatic intracranial malignancy using standard MRI can be challenging. However, MRI remains the preferred radiologic method for diagnosis and differentiation [5]. Moreover, it is important that imaging in immunocompromised patients may lack ring-enhancing regions and vasogenic edema may be less prominent than in immunocompetent patients [3]. It is imperative to differentiate an abscess from other medical conditions including meningitis and tumors, even though they may appear clinically similar, require distinct treatment, and bring distinct consequences. Brain scans using diffusion-weighted magnetic resonance imaging can assist in localizing the lesion and distinguishing between malignant tumors and ring-enhancing lesions resulting from brain abscesses [6].
Before beginning any antimicrobial treatment, stereotactic aspiration of a minimum of one lesion should be performed after brain imaging with contrast, preferably magnetic resonance imaging. It is important to handle brain abscess samples as best as possible in order to ensure accurate microbiological reporting [7]. In individuals without a serious illness, antibiotics may be delayed until the brain abscess is aspirated or excised if neurosurgery can be completed in a reasonable amount of time, ideally within less than 24 hours. The most appropriate empirical antimicrobial therapy for community-acquired brain abscess in immunocompetent people is a 3rd-generation cephalosporin and metronidazole, with trimethoprim-sulfamethoxazole and voriconazole added in patients with severe immunodeficiency. Carbapenem coupled with vancomycin or linezolid is the recommended empirical treatment for a post-neurosurgical brain abscess. The recommended course of antibiotic therapy is 6–8 weeks. There is no suggestion for early transition to oral antibiotics due to a lack of data. Adjunctive glucocorticoid medication is helpful for severe symptoms caused by perifocal oedema or imminent herniation. Primary antiepileptic prophylaxis is not advised [8]. The preferred course of treatment for an abscess is still surgical excision or drainage followed by a long-term course of antibiotics (typically, 4–8 weeks) [9].
It is essential to address the infectious source quickly in order to avoid the fatal prognosis that comes with brain abscesses. One study verifies the relevance of the Glasgow Coma Scale (GCS) and comorbidities as predictive factors and provides encouraging data on the safety of using an oral switch for antibiotic treatment of brain abscess. The oral switch could reduce catheter-induced iatrogenic problems and improve the patients’ quality of life [10]. Early diagnosis of a brain abscess increases chances of survival and lowers the fatality rates.
This comprehensive case report emphasizes the necessity for clinicians to remain cautious in recognizing potential risks of brain abscess, especially in immunocompromised patients. The ever-evolving array of therapy options highlights the ongoing efforts to improve the management of this illness. In the future, multicentric prospective research should be conducted to gather more evidence concerning brain abscess management. In immunocompetent individuals, the best empirical antibiotic therapy for a community-acquired brain abscess is a combination of metronidazole and a third-generation cephalosporin, whereas, in patients with severe immunodeficiency, trimethoprim-sulfamethoxazole and voriconazole should be added.